Is physical therapy covered by insurance
Is physical therapy covered by insurance
Physical therapy is one of the health care services that every injured, sick, or post-surgery person needs to undertake. They definitely affect beneficiaries’ independence, uneasiness, and overall well-being for beneficiaries who obtain home modifications. However, the cost of physical therapy can be a concern, departure many to wonder: Is physical therapy covered by insurance? This article aims to answer this important question and to give you a rapid of what this guide will do to help you make the right decision relating to your insurance policy concerning your health care.
What is physical therapy covered by insurance?
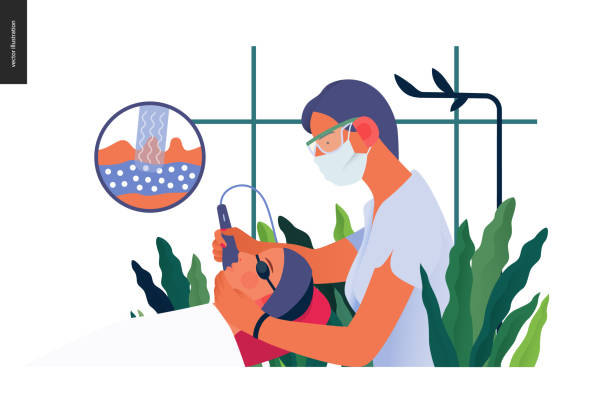
Physiotherapy (PT) can thus be defined as a healthcare profession that utilizes physical methods to bring back, sustain, and enhance movement and functional ability. Taking into consideration the facts related to the case of the patient, physical therapists analyze the necessity of certain actions in particular patients and give the direction that should be undertaken to achieve the goals set. It can be useful in the following situations: when the patient has surgery; when the patient is in acute pain; and during a long-term disease.

Of course, there are a lot of benefits of PT, but knowing costs, specifically insurance, is knowledge that will serve to introduce actual care.
Is physical therapy covered by insurance?
The good news, however, is that the common of insurance plans do allow physical therapy; however, the extent and circumstances under which the physical therapist can perform the process are normally a topic of discussion. If you are an insured person, you will be in a position to discover that the health insurance policy will differ from policy to policy or from your private health insurance to Medicare and Medicaid if you own one. Here’s a breakdown of common factors swaying coverage:
Type of Insurance Plan
Private Health Insurance:
Many private insurance organizations include physiotherapy services in their ordinary package of convenience. However the therapy might not be straight accessible to the patient, and the patient may require a referral from the doctor for the therapy, or the patient may require approval for the therapy.
Medicare:
This means Medicare Part B will pay for physical therapy services that are brought outside a hospital if the PT feels that they are medically needed. We know it usually requires a certified plan of care from your physician.
Medicaid:
These state Medicaid plans are different but commonly provide physical therapy to those clients, especially needy ones below the EPSDT benefit.
Medical Necessity
It was also found that most insurance providers only allow for reimbursement for PT if it is considered a medical necessity. It therefore has to meet a certain health requirement, like treatment after surgery or a chronic disease.
Out-of-Pocket Costs
Even with insurance, you may face some out-of-pocket expenses like:
- Deductibles: The amount of money that the policyholder has to spend before they can make a policy claim.
- Co-pays: A fixed fee per session.
- Co-insurance: Any part of the cost which you are required to bear.
Session Limits
Some plans set annual or monthly caps on the number of times the individual may see a physical therapist. When one has such basic working knowledge, unnecessary overruns or other extra costs that would be overlooked will be avoided.
Signs That Your Physical Therapy Is Covered by Insurance
Understanding your insurance coverage can feel overwhelming, but a few steps can make the process simpler:
Insurance Information you also have to find out from the insurance documents whether the insurance company covers physical therapy or not. Searches that use the words “rehabilitation services,” “therapy,” or the word “benefits” should be attempted.
Ensure that you communicate with your insurance service provider. Whether it is an insurance company, self-funded, or fully funded insurance plan, ensure that you take your time and reach out to your insurance service provider. Ask questions like:
- Is physical therapy covered by insurance under my current plan?
- Are there any pre-authorizations?
- What does this mean to me, or even better, what will be my out-of-pocket expenses?
Phone Your Physical Therapist Many PT offices assist with insurance eligibility. They should enable you to establish which services will be of benefit and the expense that you will be charged.
Ways to Get Close to or Go Over the Insurance Limits on Physical Therapy
Navigating insurance for physical therapy can be challenging, but these tips can help you get the most out of your coverage:
Contact Doctor Although you do not have to do so, a letter from a doctor emphasizes the expediency of medical necessity.
Choose in-network providers. With in-network physical therapist straps, you may be able to spend a lot less.
Usual Pre-Authorization Requirements Some insurers will require authorization before they begin your treatment. Its absence may lead to such a state when certain claims will not be paid at all.
If your insurance offers the maximum number of sessions that it will cover, you should monitor the sessions to avoid further bills.
Below are the steps to take if your insurance claim is rejected. Appeal Denied Claims If an insurance company has rejected your insurance claim, there might be a chance that you appeal that decision. All documents that can be needed to support the narration of the case should be provided.

Personal research, specifically the revelation of insurance approvals when it comes to physical therapists
While many insurance plans offer coverage, there are common obstacles, including:
Limited Coverage for Preventive Care:
Actually, some of those policies do not include physical therapy for preventive care when the same may be helpful in preventing further misfortunes in the future.
High Out-of-Pocket Costs:
This means even for serious illness treatment becomes very costly when one has to pay for his/her portion of the bill in the form of deductibles or co-pays.
Complex Approval Processes:
The preauthorization and documentation process also barred the initiation of therapy.
Knowing these should assist you to better prepare yourself and not be caught off guard.
Conclusion about is physical therapy covered by insurance
So, is physical therapy covered by insurance? Operatively, yes, but the terms will vary with your policy and the conventions regarding your condition, in terms of whether it comes with session-number restrictions or other forms of prior authorization. As a result, analysis of the medical insurance policy gives an understanding of the types of services provided by the insurer and leads to a reduction of costs by the consumer.
It is therefore important to embark on physical therapy for your health’s sake, and the right information will make you weigh the cost and options. Do not just take things lying low with your caregivers, and ensure you look for ways that will allow you to get the best care.
FAQs about is physical therapy covered by insurance
What about physical therapy? Is Medicare a requirement?
Indeed, Medicare Part B does provide reimbursement for outpatient physical therapy services, provided that the services offered are medically necessary. This will depend on a doctor’s plan of care.
What are the ways that I can minimize the expenses of part-paying the physical therapy treatments?
To keep costs down, see network doctors, and if necessary, ask your therapist if your insurance is limited for payment options or if a pre-authorization is required.






